Combo of cabozantinib plus atezolizumab active across kidney cancer subtypes
September 9, 2021 By Gregor Kreth
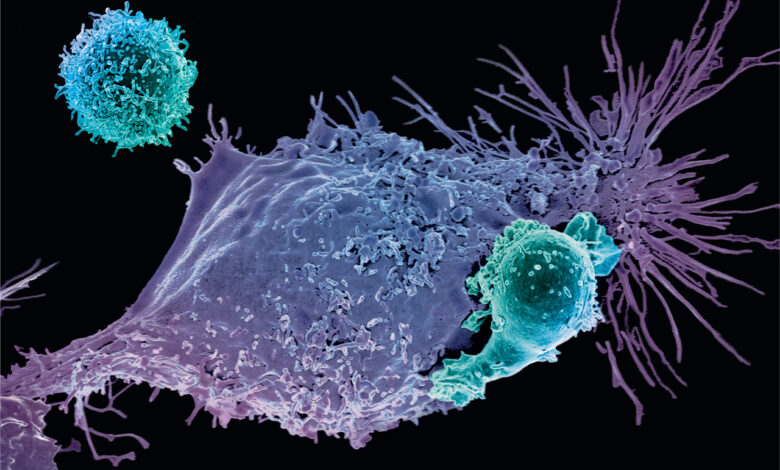
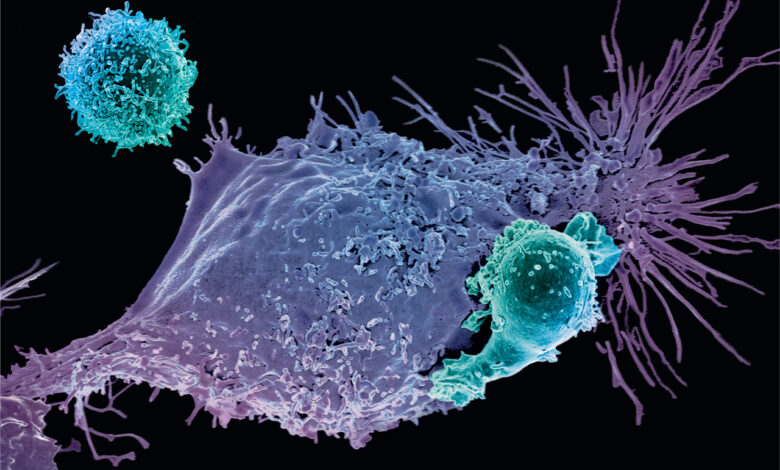
Recent findings based on the phase 1b COSMIC-021 trial in Journal of Clinical Oncology demonstrated that treatment with the multikinase inhibitor cabozantinib (Cabometyx) plus the immune checkpoint inhibitor atezolizumab (Tecentriq) showed promising efficacy in patients with both clear cell (cc) and non–clear cell (ncc) renal cell carcinoma (RCC), according to findings from the phase 1b COSMIC-021 trial.1 The combination reached an objective response rate (ORR) as high as 58% across two ccRCC cohorts and an ORR of 31% in patients with nccRCC.
“Cabozantinib plus atezolizumab demonstrated encouraging clinical activity in patients with advanced RCC regardless of histology. The safety profile with the combination was tolerable with dose modification and comparable to previous reports,” first author Sumanta K. Pal, clinical professor, Department of Medical Oncology & Therapeutics Research; co-director, Kidney Cancer Program, City of Hope, and coinvestigators wrote.
The multicenter, open-label phase 1b COSMIC-021 trial (NCT03170960) enrolled 102 patients with advanced RCC. Patients with ccRCC received atezolizumab plus either 40 mg (n = 34) or 60 mg (n = 36) of cabozantinib. Patients with nccRCC (n = 32) received atezolizumab plus 40 mg of cabozantinib.
In the 40-mg cabozantinib ccRCC group, the median age was 68 (range, 39-87), 79% of patients were male, and 71% were White. The ECOG performance status was 0 for 79% of patients and 1 for 21% of patients. Regarding IMDC risk, 21% were favorable, 76% were intermediate, and 3% were poor. Twenty-six percent of the cohort had a sarcomatoid component, which was significantly higher than the other 2 study arms. The PD-L1 status by CPS was ≥1 for 26% of patients, <1 for 44% of patients, and unknown for 29% of patients. Fifty-three percent of patients had ≥3 tumor sites. Metastatic sites included lung (79%), lymph node (47%), liver (15%), and bone (12%). One patient had received prior systemic anticancer therapy, 3 patients had prior radiotherapy, and 85% of patients had prior nephrectomy.
In the 60-mg cabozantinib ccRCC group, the median age was 60 (range, 42-82), 72% of patients were male, and 94% were White. The ECOG performance status was 0 for 69% of patients and 1 for 31% of patients. Regarding IMDC risk, 39% were favorable, 58% were intermediate, and 3% were poor. Six percent of the cohort had a sarcomatoid component. The PD-L1 status by CPS was ≥1 for 22% of patients, <1 for 50% of patients, and unknown for 28% of patients. Thirty-nine percent of patients had ≥3 tumor sites. Metastatic sites included lung (75%), lymph node (42%), liver (8%), and bone (11%). One patient had received prior systemic anticancer therapy, 4 patients had prior radiotherapy, and 89% of patients had prior nephrectomy.
In the nccRCC group, the median age was 62 (range, 37–78), 81% of patients were male, and 72% were White. The ECOG performance status was 0 for 75% of patients and 1 for 25% of patients. Regarding IMDC risk, 38% were favorable, 47% were intermediate, and 16% were poor. Thirteen percent of the cohort had a sarcomatoid component. Regarding histology subtype, 47% were papillary, 28% were chromophobe, and 22% were others. The PD-L1 status by CPS was ≥1 for 13% of patients, <1 for 56% of patients, and unknown for 31% of patients. Fifty-six percent of patients had ≥3 tumor sites. Metastatic sites included lung (50%), lymph node (59%), liver (16%), and bone (16%). Seven patients had received prior systemic anticancer therapy, 2 patients had prior radiotherapy, and 69% of patients had prior nephrectomy.
The median follow-up for the 40-mg ccRCC arm was 25.8 months and the ORR was 53%, including a complete response (CR) rate of 3%. The median progression-free survival (PFS) was 19.5 months. In the 60-mg ccRCC arm, the median follow-up was 15.3 months and the ORR was 58%, including an CR of 11%. The median PFS was 15.1 months. Among patients with nccRCC, the ORR was 31%, comprising all partial responses. The median PFS was 9.5 months.
Regarding safety, grade 3/4 treatment-related adverse events (TRAEs) occurred in 71% and 67% of patients in the 40-mg and 60-mg ccRCC groups, respectively. TRAE-related discontinuation of both drugs occurred in 15% and 6% of these 2 arms, respectively. In the nccRCC arm, 38% of patients had grade 3/4 TRAEs and TRAEs led to discontinuation of both drugs in 3% of patients. No treatment-related death occurred in the trial.
“These results support further evaluation of cabozantinib plus atezolizumab in patients with advanced RCC in the phase III trial setting, including those with non–clear cell histology. Patients with non–clear cell RCC have limited treatment options, and prospective data on tyrosine kinase inhibitor plus immune checkpoint inhibitor combinations are lacking for this population,” the authors wrote.
Reference
1. Pal SK, McGregor B, Suárez C, et al. Cabozantinib in combination with atezolizumab for advanced renal cell carcinoma: results from the COSMIC-021 study [published online ahead of print September 7, 2021]. J Clin Oncol. doi: 10.1200/JCO.21.00939